INTRODUCTION
Rapid eye movement (REM) sleep behavior disorder (RBD) is a sleep disorder characterized by dream-enactment behavior (DEB) and REM without atonia (RWA) [1]. RBD causes sleep disruption and trauma to the patient and/or bedpartner during sleep [1,2].
The standard treatment for RBD is the maintenance of a safe bedroom environment and medications, including clonazepam, immediate-release melatonin, and pramipexole [2,3]. In most cases, complex motor symptoms and violent behaviors are well controlled with medical treatments [2,3]. However, a few patients with RBD are medically intractable and even have secondary problems, including major injuries [2,3].
Obstructive sleep apnea (OSA) is a highly prevalent sleep disorder that presents recurrent upper airway collapse during sleep, and many patients with RBD have comorbid OSA [1,4,5]. Although OSA is common in patients with RBD, the influence of comorbid OSA on RBD symptoms remains unclear [4-6]. A previous report showed OSA, especially in highly severe cases, might mask the symptoms of RBD by reducing REM sleep duration and REM sleep fragmentation [7]. However, other studies suggest OSA may exacerbate complex motor behavior in patients with RBD by increasing arousal after respiratory events and sleep fragmentation [4,5,8]. In addition, several studies suggested OSA treatment with continuous positive airway pressure (CPAP) improved RBD symptoms and RWA on night polysomnography (PSG) [4,5].
Here, we discuss a case of medically intractable RBD that was diagnosed as concomitant OSA by 10-year follow-up PSG and was treated successfully with CPAP therapy.
CASE REPORT
A 69-year-old male visited a sleep clinic with abnormal behavior during sleep. He was sleeping, talking, and yelling, depending on his dreams. He complained of aggressive behavior, including punching and kicking, during sleep and had a history of minor trauma to his hands and feet. The patient did not complain of snoring or cognitive function problems. He had no medical history and was not taking any medication; however, he had been drinking a bottle of Makgoelli daily for 10 years. The patient’s body mass index (BMI) was normal (24.1 kg/m2) and had no craniofacial abnormalities (Mallampati grade 2). A neurological examination revealed no signs of Parkinsonism.
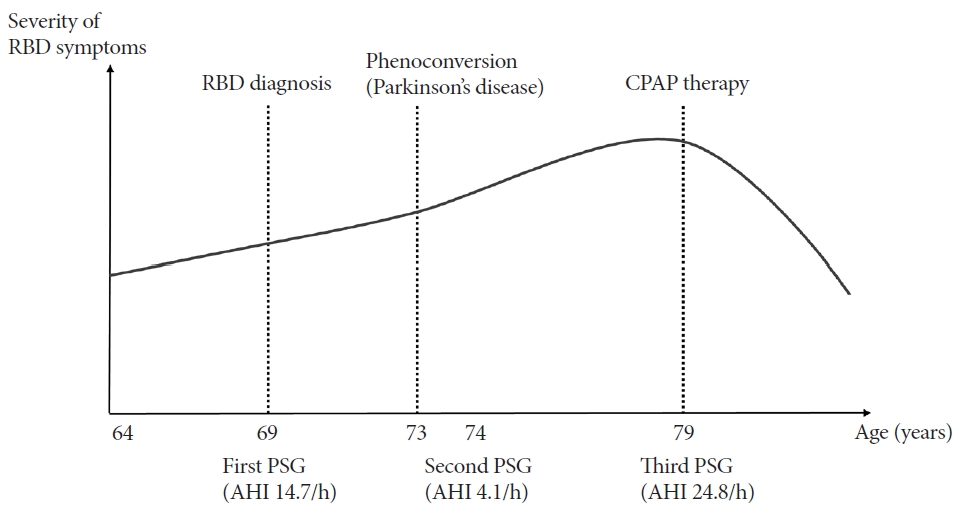
In-lab night PSG was performed and scored following the American Academy of Sleep Medicine guidelines [9]. The total sleep time (TST) was 331.0 minutes (min), and REM sleep was observed at 70.0 min (21.1% of the TST). A night-time PSG showed RWA with DEB, including punching, sleeptalking, and yelling. In addition, mild OSA with an apneahypopnea index (AHI) of 14.7/h and heavy snoring were observed. The patient had frequent arousal, with an index of 25.2/h, mostly related to respiratory events (respiratory-related arousal, 13.3/h).
Although mild OSA was demonstrated in the first PSG, medical treatment for RBD was preferred over OSA because oxygen desaturation was not significant and the patient did not have clinical symptoms of OSA. Medical therapy with clonazepam was initiated, and a clinician informed the patient regarding safe bedroom environments and recommended stopping alcohol consumption. However, the severity of excessive motor behavior during sleep worsened, and he experienced several minor injuries due to the RBD symptoms. We tried other medications, including high-dose clonazepam (1.5 mg daily), immediate-release melatonin (5 mg daily), and pramipexole (0.25 mg daily). However, his symptoms remained despite the medical treatment.
Four years later, the patient developed tremors, slow movement, and gait disturbances. Neurological examination revealed resting tremors, rigidity, and bradykinesia, suggesting idiopathic Parkinson’s disease. Medical treatment with levodopa-carbidopa was initiated while maintaining RBD medications. One year after being diagnosed with Parkinson’s, his RBD symptoms persisted, and his bed partner reported severe snoring. The second follow-up PSG was performed; the patient did not take RBD medication on the day of the PSG.
In the second PSG, the TST was 509.5 min, and REM sleep was observed at 130.5 min (25.6%). RWA was observed in 45.6% of the total REM sleep, and DEB with punching and kicking movements was observed during REM sleep. Moderate snoring was observed, but only a few respiratory events were within the normal range (AHI 4.1/h). Arousal and sleep efficiency were within the normal ranges.
Medical therapy was continued, and since the RBD symptoms worsened and became intractable, the medications were increased to high doses (clonazepam 1.5 mg daily; immediate release, 10 mg daily; and pramipexole, 1.375 mg daily). After another 5 years, his symptoms worsened, and he broke a window and punched his bedpartner during sleep. The patient presented with excessive daytime somnolence, and his bedpartner witnessed severe snoring and apnea during sleep. The patient did not show a significant change in body weight (BMI 24.3 kg/m2). Follow-up PSG is recommended to differentiate between comorbid OSA and RBD. He did not take RBD medications on the day of PSG.
In the third PSG, TST was 298.0 min, and REM sleep was observed at 104.5 min (35.1%) (Fig. 1A). RWA was observed in 79.9% of the total REM sleep, and DEB with punching and kicking movements was observed during REM sleep (Fig. 1B). In addition, the third PSG showed moderate OSA, with an AHI of 24.8/h and heavy snoring. The lowest O2 saturation level was 90% after a respiratory event. The patient experienced frequent arousal during the study period (arousal index, 35.6/h), mostly related to respiratory events (respiratory-related arousal, 21.3/h) (Fig. 1C).
The patient started to use auto-CPAP at a pressure of 5–15 cmH2O, maintaining RBD medications. The patient complied well with the auto-CPAP therapy and used a CPAP machine for 6 h daily. After one month, his violent behavior during sleep resolved, and he only had mild remnant sleep-talking symptoms. He had been consistently using auto-CPAP without reporting a recurrence of RBD symptoms for 6 months. The RBD medications were continued concurrently, but the dose of clonazepam was reduced due to drowsiness. The patient’s clinical course is shown in Fig. 2.
DISCUSSION
This patient presented with medically intractable RBD, in which OSA was not initially detected, and was diagnosed with comorbid OSA by a 10-year follow-up PSG. The RBD symptoms improved with nasal CPAP therapy.
Although not clearly understood, several previous reports suggest sleep-disordered breathing could aggravate RBD symptoms and that CPAP therapy could improve the symptoms [4-6,8]. One reason is that severe OSA can mimic RBD symptoms, which is called “pseudo-RBD. [6,8]" Patients with severe OSA can present abnormal behavior upon arousal after respiratory events, which may appear similar to DEB in RBD [6-8]. In cases of true RBD comorbid with OSA, DEB symptoms could be improved with CPAP therapy by reducing pseudo-RBD behaviors related to respiratory events [4-6]. In addition, severe OSA causes sleep fragmentation and frequent arousal [5,6]. Recent studies indicate that brainstem control of limb muscle activity is closely related to the motor symptoms of RBD [6]. Since OSA causes recurrent cortical microarousal, it may contribute to brainstem activation with increased muscle activity, exacerbating RBD symptoms [5,6]. In this case, the last PSG showed moderate OSA with frequent respiratory-related arousal. CPAP therapy may decrease arousal by preventing respiratory events, thus improving the motor symptoms of RBD.
In addition, the finding of this case is that moderate OSA was demonstrated in the follow-up PSG after 10 years but was not observed in the first and second PSG. The cause of worsening respiratory events in the follow-up PSG was thought to be most closely related to aging. Aging is known as an important risk factor for OSA [10]. Older age is associated with increased upper airway collapsibility, independent of sex and BMI, by decreasing the reflex function of respiratory muscles [10]. In this case, as other risk factors for OSA, including BMI, did not change for 10 years, it can be assumed that moderate OSA might develop with aging.
In this case, RBD worsened due to OSA, and the complex motor symptoms of RBD improved with CPAP treatment. Based on their medical history, it is important to perform PSG on patients suspected of having RBD to diagnose coexisting sleep disorders, including OSA. In addition, even if there are no other sleep disorders in the initial PSG, follow-up PSG should be considered to diagnose comorbid OSA if the symptoms worsen or are medically intractable. Clinicians should be aware of concomitant OSA when patients have intractable RBD symptoms, and CPAP therapy may help improve RBD symptoms.