AbstractObjectivesTo compare night-time muscle activity in children with cerebral palsy (CP) with that in typical developing peers.
MethodsPolysomnography with electroencephalography (EEG), electrocardiogram, electromyography (EMG), respiration, and electrooculography movements recorded during one night were used to characterize sleep stages in a group of children with CP (Gross Motor Function Classification Scale I–III) and a group of typically developing (TD) children (aged 3–13 years). Periods of EMG activity for the tibialis anterior and soleus (SOL) muscles were identified, and the coherence between EEG and EMG was measured to assess corticomuscular drive during sleep.
ResultsThere were no significant differences between the groups in total sleep time, average time spent awake, or rapid eye movement, N1, and N3 sleep. Children with CP spent significantly less time in N2 than their healthy peers (43% vs. 51%, p=0.03). There was only a significant difference between TD and CP in SOL muscle activity during the wake stage. Otherwise, there were no differences between groups in coherence in EEG and EMG signals for any sleep stage.
ConclusionMildly affected children with CP do not show altered night sleep or muscle activity patterns as compared to TD peers. Abnormal muscle activity is unlikely to contribute to sleep disturbance, development of contractures, joint deformation, pain, or general discomfort in this group of children with CP.
INTRODUCTIONCerebral palsy (CP) is caused by a disturbance in early neural development prior to or during birth [1]. The main characteristic affected is motor development, but cognitive, perceptual, and emotional challenges are also frequent.
Sleep disturbances are also frequent in children with CP, with estimates ranging from 13% to 85% [2,3]. These sleep disturbances have been shown to greatly affect quality of life [4-8] and negatively impact school-performance [9-11].
The cause of sleep disturbances in children with CP is unclear and likely multifactorial. Involuntary muscle activity in the form of spasticity, dyskinesia, and dystonia is likely to affect sleep, although a recent study using motion tracking found reduced movements during sleep in children with severe CP (Gross Motor Function Classification Scale [GMFCS] level V) as compared to typically developing (TD) peers [12]. Activity in individual muscles, especially in the form of increased (static) muscle tone, may go undetected in gross motion tracking and requires EMG monitoring throughout the different sleep stages.
Information about the activity levels of individual muscles is also important to clarify whether increased night-time muscle activity contributes to contractures and joint displacements. Many children with CP wear orthoses during the night because they are thought to prevent contractures and joint deformities by maintaining the joint in a neutral position despite involuntary muscle tone [10,13,14]. Night orthoses have the advantage that they do not interfere with daily activities, but they are associated with discomfort and, in all likelihood, disturb sleep [15]. Therefore, they may add further to the existing sleep disturbances. There is also an ongoing debate on whether muscle contractures are related to muscle overactivity (increased muscle tone) or reduced muscle activity and growth [16,17]. Clarifying whether children with CP show more or less night-time muscle activity than other children may also help inform this debate.
Therefore, the primary purpose of the present study was to evaluate muscle activity during various sleep stages in children with CP and TD peers. We hypothesized that children with CP would show more frequent and longer-lasting episodes of muscle activity compared with TD children. We included measures of corticomuscular coherence (CMC) and intermuscular coherence (IMC) to indirectly assess the functional connectivity of the corticospinal tract. CMC is an established method to assess a neurophysiological marker of functional coupling between the primary motor cortex and the contralateral limb18,19 as well as the coupling of neural signals to different muscles. The CMC between electroencephalography and electromyography (EEG-EMG) and the IMC between EMG-EMG signals reflect the common oscillatory drive to motor units from the corticospinal tract based on the frequency and time (synchronicity) domains [14]. Research has shown that beta-band frequencies are the most dominant during muscle contractions. However, CMC is greatly reduced in subjects with lesions in the central nervous system [20,21]. Decreased CMC has been associated with a lower cortical drive to the contralateral muscles, which subsequently affects ongoing motor control and hence sensorimotor development [22]. Whether the sleep architecture and the concurrent functional CMC or IMC differ between children with CP and TD children has not been investigated. This could have an impact on the night-time muscle activity. Animal research supports an altered night-time CMC pattern during certain sleep stages depending on animal health and related to neurodegenerative diseases [23,24]. Although CP is not a neurodegenerative condition, CMC patterns are affected during active movements, which could be affected during sleep.
Therefore, the secondary purpose of the study was to use CMC and IMC to investigate possible altered neural activation in children with CP as compared to TD peers at different sleep stages.
METHODSSubjectsTwelve children (9 boys, 3 girls) diagnosed with CP in the age range between 3–13 years (average age: 8.7±3.6) and a control group of 15 TD children aged 4–13 years (10 boys, 5 girls; average age: 9.0±3.1) were included in the open-label exploratory study. Only children diagnosed with spastic CP and a functional level of I–III according to the GMFCS [25] based on their medical records were included. We did not collect information regarding the use of night-time orthoses. The children included in the study and diagnosed with CP did not report any sleep disturbances, as these were not part of the inclusion criteria. Since our main focus was to evaluate muscle activity and corticospinal tract activity, we did not include subjective reporting on sleep disturbances. Children who received muscle relaxants or sleep medications were excluded. Muscle tone was clinically evaluated according to the Modified Ashworth Scale (MAS) [26] as part of an initial neurological examination (Table 1).
All children were recruited from the Greater Copenhagen area in Denmark. All legal guardians received written and verbal information about the study, and prior to the experiment, they signed an informed consent form for their child to participate in the study. Afterwards, participants were offered a gift to show appreciation for their participation in the study.
The study was approved by the local ethics committee (H-16019427), and all procedures conducted in accordance with the standards of the Helsinki Declaration.
MaterialsWe used polysomnography (PSG) to record a single night of sleep in children’s natural surroundings according to the accepted guidelines from the American Academy of Sleep Medicine (AASM) [27]. A custom-made montage was used to record the EEG from electrodes placed on F3, F4, C3, C4, O1, O2, M1, M2, and Cz (as reference) (Ambu 72620-M, Ballerup, Denmark) using the 10–20 system, right and left electrooculography (EOG), bipolar submental EMG (Ambu 72020-K), electrocardiogram (ECG), thoracic and abdominal excursions (piezo bands), oxygen saturation with a pulse oximeter sensor (Nonin Medical, Playmouth, MN, USA), nasal airflow (Pro- Tech, Murry Ridge Lane, Murrysville, PA, USA), and bilateral EMG muscles. All measurements were recorded using a transportable ambulatory EEG/polygraph TrackIt 3.0- device with the following dimensions: 14×9.5×3 cm (Lifelines Neuro, Nr. Stockbridge, Hants, UK).
In the following data analyses, we chose to focus only on the tibialis anterior (TA), soleus (SOL) muscles, as this allowed us to investigate the affected muscles in children with both hemiplegic and diplegic CP. These muscles were chosen because they are both well studied in children with CP. Furthermore, spasticity is known to mainly affect the ankle plantar flexors, whereas ankle dorsiflexors are often paretic in children with CP [17,28].
Experimental designIn the late afternoon of the day preceding the night of recording, the child and its caregivers visited the laboratory at the Elsass Foundation (Charlottenlund, Denmark) where the initial neurological examination was performed, and the equipment mounted on the child. The skin over the bilateral TA, SOL, deltoideus, lateral eye muscles, and chin muscles was prepared using a skin prep (3M Red Dot). TA, SOL and deltoideus data were obtained from paired monopolar recordings; data from the other muscles were obtained from bipolar electrode recordings. Electrodes were placed 2 cm apart on the bellies of the respective muscles. Electrodes were placed to monitor the heart. The skin on the scalp was prepared using Nuprep gel (Weaver and Company, Aurora, CO, USA). EEG electrodes were attached to the head using a Ten20 conductive electrode paste (Weaver and Company). All electrodes were placed as indicated in Fig. 1, and attached close to the body surface, running under the clothes, and collected behind the neck before plugging the cable in the transportable ambulatory EEG/polygraph TrackIt-device. The cables were placed so that they could change their clothes, if necessary. Thoracic and abdominal belts were placed afterwards, and their cables attached to the bundle of cables from the electrodes. Parents and children were instructed on how to attach the nasal airflow and how to place the oxygen saturation device on the child; this procedure could either be performed just prior to falling asleep or when the child was already asleep to minimize discomfort. The TrackIt-device was placed in a small backpack easy to carry. The families were instructed on how to carry the bag during the rest of the day and how to handle it during the night. The experimental setup did not exclude the child from regular daily activities, except for water activities.
During mounting, the TrackIt-device was connected to a computer, which allowed online monitoring of the signal quality of all electrodes and respiration belts when the child was asked to contract specific muscles and to take deep breaths using the Nicolet Nervus software (Natus 5.94 Neurology Inc., Middleton, WI, USA). After an online signal quality check, the TrackIt-device could be detached from the computer. The device sampling rate was 200 Hz. The sleep recording was controlled to start just prior to the regular child bedtime based on approximate hours provided by the parents. Parents and children were asked to follow regular bedtime hours despite the attached equipment. Furthermore, they were instructed to note the time when the child went to bed and woke up. As a final instruction, they were explained how to detach the equipment the following morning. Data were saved locally on the Track- It-device until the equipment was returned to the researchers for offline data analysis.
AnalysisSleep registrationTwo independent raters performed offline sleep scoring based on 30 second epochs according to the AASM manual for the scoring of sleep and associated events [27]. Hypnograms were based on the sleep recording analysis, where each sleep stage was characterized as follows: wake, rapid eye movement (REM), N1, N2, and N3. The total amount of sleep was calculated by the hypnograms in minutes, lasting from the first indication of N1 until the first notation of W not followed by any sleep stages. The time in bed was also recorded in minutes.
EEG and EMG preprocessingRaw EEG and EMG data were transferred to MATLAB (ver. R2015a, MathWorks, Natick, MA, USA) for further EMG and EEG analyses. The recorded EDF files from the TrackIt-device were then processed in EEGlab (v. 14.1.1b, Swartz Center for Computational Neuroscience, San Diego, CA, USA) to calculate EMG activity from the TA and SOL muscles and performing CMC analyses between the Cz electrode and TA and SOL muscles, respectively. We chose Cz because this electrode placement corresponds well with the distal leg area of the motor cortex for both the right and left legs. Because the Cz electrode was recorded as reference electrode, a new reference was initially calculated as the average of the F4, F3, O2, O1, C4, C3, and the Cz electrode was then re-referenced to the new average reference. The Cz electrode signal was high-pass filtered with a cut-off of 0.5 Hz and notch filtered between 45– 55 Hz to remove line-noise. Finally, the signal was downsampled to 128 Hz. For the four lower limb muscle signals, that is, bilateral TA and bilateral SOL, the paired monopolar recordings were re-referenced to obtain four bipolar signals. These were then high-pass filtered with a cut-off of 5 Hz and notch filtered between 45–55 Hz to remove line-noise. Cz and EMG signals were then exported as .set files for further processing using custom MATLAB scripts.
EMG activityBased on the offline sleep analyses, periods with artefacts due to loose electrodes or similar problems were excluded from further analysis. This corresponds to an average EMG data inclusion of 91.9%±7.8 and 93.6%±4.7, for the CP and TD groups, respectively, based on measures from TAright/TAleft and SOLright/ SOLleft. EMG signals were rectified, and the mean EMG activity across the whole night calculated for each muscle. Further EMG data processing was performed separately for the different sleep stages and for each muscle. EMG activity bursts were defined as EMGs exceeding the mean EMG activity+1SD of the whole night EMG activity for each muscle. Based on the total time spent in each sleep stage, we then calculated the total time and sleep stage fraction where EMG activity exceeded the mean+1SD. For subsequent coherence analyses, we only performed coherence analyses when the EMG activity exceeded the mean+1SD EMG activity.
Intermuscular and corticomuscular coherenceThe magnitude squared coherence (C) at frequency (λ) analyses was performed using the Neurospec 2.0 toolbox for MATLAB, calculated using the formula
Coherence quantificationTo quantify coherence in the beta band, coherence >95% confidence interval (CI) was summed from 15–30 Hz. If coherence measurements were <95% CI, 0 was added to the sum. Coherence can take any value between 0 and 1, but the summed coherence can be higher than 1.
Least/most affected sideWe tested the least and most affected side of children with CP. To this effect, we used the MAS score of the ankle joint. If the MAS score did not uniquely determine the most affected side, the separation of the least and most affected side in children with CP was based on their preferred hand, as this was also their less impaired side. For TD children we used the average of the left and right side of muscle activity for further analysis since no difference was found between the two sides: neither TA nor SOL EMGs, respectively (F1,25=0.00246, p=0.961 and F1,25=0.456, p=0.512).
Statistical analysesStatistical analyses were performed using the software package R (R-studio, version 1.3.959, R-version 4.0.2 [2020-06-22]).
Analysis of total sleep time followed a general linear model with group (CP or TD) as the independent fixed effect together with Age and Sex. Inference was subsequently tested for differences between the two groups.
Analyses of sleep time at each sleep stage followed a linear mixed model. Group-by-Sleep stage was tested as the independent fixed effect, and age, sex, and GMFCS score were included as fixed effects, and participants as random effects. We then tested the linear differences between the two groups for each of the five sleep stages. Significance was assessed after Bonferroni correction for five comparisons.
Analyses of TA activity, SOL activity, TA-SOL coherence (IMC), Cz-TA coherence, and Cz-SOL coherence (CMC) at each sleep stage followed a linear mixed model. Group-by-Sleep Stage-by- Affected Leg was tested as independent fixed effect, age, sex, and GMFCS score were included as fixed effects and participants as a random effect. We then tested the linear differences within the CP group (least affected vs. most affected) and between the CP and TD groups, both (least affected vs. average and most affected vs. average) for each of the five different sleep stages. Significance was subsequently assessed after Bonferroni correction for 15 comparisons.
RESULTSTotal sleepThe total sleep time during the night was, on average, 574.75± 99.1 min (9.58±1.65 h) for children with CP while children in the TD group spent an average of 572.73±45 min (9.55±0.75 h). The fitted GLM: Total Sleep Time Group (TD, CP)+Age+Sex revealed a significant effect of age (t=-3.777, p=0.000978), that is, increasing age was negatively correlated with total sleep time. The comparison between the two groups did not reveal any significant differences between the CP and TD groups (zscore= 0.066, p=0.947).
Time in sleep stagesThe analysis of the time spent in different sleep stages (calculated in minutes) followed the linear mixed model:
Sleep Time in Stage = Group-by-SleepStage-1 + Age + Sex + GMFCS + (1|Participant)
We did not find any significantly different sleep stage between the two groups, except for sleep stage N2 (p=0.01) (Fig. 2).
EMG activityAnalysis of the TA activity 1SD above the average activity spent in the different sleep stages followed the linear mixed model (Table 2):
TA activity = Group-by-SleepStage-by-Affected leg-1 + Age + Sex + GMFCS + (1|Participant)
Comparing the TA activity fraction revealed no significant differences in any of the linear hypotheses tested comparing the groups, affected leg, and different sleep stages.
The analysis of the SOL activity 1SD above average activity spent in the different sleep stages followed the linear mixed model:
SOL activity = Group-by-SleepStage-by-Affected leg-1 + Age + Sex + GMFCS + (1|Participant)
Comparing the fraction of SOL activity above 1SD of mean SOL activity revealed no significant differences in any of the linear hypotheses tested comparing the groups (p>0.05), affected leg, and different sleep stages, with the exception of the comparison of CP children’s most affected leg and TD children’s average activity during the wake stage and the comparison of children with CP’s least and most affected leg during the wake stage (p values are 0.021 and 0.002, respectively). In both comparisons, children with CP’s most affected leg displayed less SOL activity during the wake stage than their least affected leg and the average activity of TD children’s legs.
Since there were no significant differences between the least and most affected sides for CP children, we pooled the bilateral data in the graphs to illustrate the difference between CP and TD (Fig. 3).
Coherence analysesBoth IMC analysis, that is, TA-SOL coherence and CMC, that is, Cz-TA/Cz-SOL coherence, followed the following linear mixed model:
TA-SOL/Cz-TA/Cz-SOL coherence = Group-by-SleepStageby-Affected leg-1 + Age + Sex + GMFCS + (1|Participant)
Comparing the IMC TA-SOL coherence revealed no significant differences in any of the linear hypotheses tested comparing groups, affected leg, and different sleep stages (Fig. 4).
Comparing the CMC Cz-TA coherence revealed no significant differences in any of the linear hypotheses tested comparing groups, affected leg, and different sleep stages.
Comparing the CMC Cz-SOL coherence revealed no significant differences in any of the linear hypotheses tested comparing groups, affected leg, and different sleep stages.
In Fig. 5 we present a representative example of a participant where we identified simultaneous activity from Cz-TA and TA-SOL, marked in red and used in the following statistical measurements, for example, frequency power, coherence, and cumulant.
DISCUSSIONWe found no major differences in sleep patterns or nighttime muscle activity between children diagnosed with mild spastic CP and TD peers, except that children with mild CP spent less time in sleep stage N2. In the wake stage during the night, children with CP displayed less SOL activity in their most affected leg compared with their least affected leg and with the average SOL leg activity of their TD peers.
The average amount of nighttime sleep for both groups was somewhat lower than that previously reported for children in the age group between 4–11 years (on average 9.9–10.5 hours of sleep per night) [29]. Despite the great variety of inter-individual sleep hours, our data correspond to the recommended total hours of sleep, which for preschool children aged 3–6 years is 10–13 hours and for school-aged children is between and 9–12 hours [30,31]. We found that children with CP generally spent a longer time in bed awake (approximately one hour more than children in the TD group). This result was calculated directly from the PSG as the sum of minutes spent in wake stages, from the onset of sleep to the first Wake stage, after which no sleep stages followed. Thus, children with CP displayed more or longer episodes during the night where they were not sleeping but still lying in bed. This could indicate that children with CP find it more difficult to fall asleep if their sleep pattern is interrupted regardless of the time compared to TD children. Problems with sleep initiation and maintenance have been previously reported in this group of children [9,11,32,33]. However, the lower total sleep time in the CP group did not reach a significant difference between the two groups. Wayte et al. [32] documented several sleep disturbances that could explain the decreased total sleep time in children with CP. It seems to be an overlooked problem with an impact on the children’s quality of life, affecting both children and families [3,8,9].
The relative time spent sleeping for the TD group seems to correspond with the sleep habits of typical elementary schoolchildren [29,34]. Even though the group of children with CP showed lower total sleep, there were no significant changes between populations when dividing sleep into the different sleep stages, except that children with CP spent less time in sleep stage N2. This may indicate that children with mild CP have a reduced ability to maintain sleep, which may influence their daily functional abilities, as suggested in a recent study by Horwood et al. [11] They found that sleep-related disturbances, for example, sleep initiation and maintenance, are present in approximately 60% of school-age children and approximately 25% of preschool-aged children with CP based on 75% of data from children with CP in the GMFCS I-III group. However, general recommendations of the amount of time healthy children and adolescents should spend in the different sleep stages during night sleep [30,35] actually confirm that all children in this study, including those with CP, reached those recommendations. The reason why we observed a decrease in the time the children with CP spent in sleep stage N2 is unknown. However, these results could have a critical impact on daily activity for this population, as sleep plays an important role in brain function, physiology, and social and psychological behavior [6,36]. Lack of non-rapid eye movement (NREM) sleep has a negative effect on memory consolidation, since it is broadly accepted that synaptic pruning takes place during NREM sleep [37].
The observation of no differences in muscle activation for TA and SOL between the two populations for any sleep stage was surprising. The only significant difference was related to SOL activity during the wake stage between children with CP and TD. Previous studies have indicated that periodic limb movements may be an important cause [4,11] of sleep disturbance in children with CP, but, despite the significant difference in our data, this result was difficult to confirm due to the small population of mildly affected children. Our calculation of muscle activity during the different sleep stages also included periodic limb movements, but not as a separate measure for actual muscle activity. We could expect that the lack of support might be due to the inclusion of a heterogeneous group of children (including hemiplegic, diplegic, and tetraplegic children), which potentially have different muscle activation patterns during the night, and which we did not observe as we pooled data from that population. We decided to not separate the data into different categories of CP diagnosis as the results would be inadequate due to the low number of children in each category.
We were also unable to confirm the observation by Sato et al. [12] of reduced night-time activity in children with severe CP. This could be likely explained by the difference in CP severity among studies, although several studies have shown no correlation between sleep disorders and motor deficit severity as based on the GMFCS [8,9].
The distinct CMC (motor cortex to contralateral TA and SOL) and IMC patterns between muscles did not show any difference between the two populations. Due to the brain lesion in the CP population, we expected an altered activity pattern in the CMC during sleep, as described by several research groups [20,21] due to the finding of altered muscle activity in SOL. Healthy changes in corticomuscular drive from the motor cortex to the muscles (due to aging) have indicated a change in cortical drive during the REM, NREM, and AWAKE sleep stages in the delta, theta, and beta frequencies, especially in the REM stage [24].
Importantly, since we only observed a significant change in SOL activity during the wake stage in children with CP compared to TD children, our results cannot confirm or reject either hypothesis regarding increased muscle activity or changes in the common neural drive.
LimitationsThe age group ranged from 3–13 years of age. This includes a variance in sleep time for children with and without CP. Although individual sleep time varies greatly among children, all children in our study reached the recommended level for sleep. In Horwood’s research, they grouped children based on age preschool and school ages [11]. Due to the small number of participants in our study, this was not possible.
We included only children with mild CP. According to other studies, children with more severe CP tend to have an altered motor activity pattern compared with children with mild CP. However, the study by Newman et al. [9] did not find any change in sleeplessness associated with the children’s GMFCS, but they did observe a tendency of full body movement caused by involuntary activity, which could influence sleep patterns. The effect of CP severity on the muscle activation pattern during sleep remains unclear, therefore, more research is needed to address this question.
ConclusionThe evidence from this study does not indicate any difference in muscle activity between children with CP compared to TD peers during sleep, except for the wake stage in SOL activity. Further, we did not find any difference in CMC or IMC in the various sleep stages between the two populations. This suggests that abnormal muscle activity during different sleep stages is not the likely cause of contracture development in children with CP. However, these results must be taken with caution because of the limited number of participants. Furthermore, we only investigated the mildest GMFSC I–III groups; therefore, we cannot completely exclude the possibility that an altered muscle activation pattern during the night can be observe in more severe CP cases. As sleep is a complex and dynamic process that reflects the specific spatiotemporal patterns of neuronal oscillations, we encourage more research on this topic to gain further information on how and when altered muscle activity patterns lead to contractures.
AcknowledgmentsWe thank all the children and their parents for their time and effort in participating in the research. We would also like to thank Jakob Skadkær Møller for his technical expertise in the setup of the equipment.
NotesAuthor Contributions
Conceptualization: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund, Jens Bo Nielsen, Troels Wesenberg Kjaer. Data curation: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund. Formal analysis: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund, Mia Dyhr Thomsen, Maria Joy Normann Haverberg. Methodology: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund, Mia Dyhr Thomsen, Jens Bo Nielsen. Project administration: Anina Ritterband-Rosenbaum, Troels Wesenberg Kjaer. Visualization: Anina Ritterband-Rosenbaum, Mark Schram Christensen. Writing—original draft: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund, Jens Bo Nielsen, Troels Wesenberg Kjaer. Writing—review & editing: Anina Ritterband-Rosenbaum, Mark Schram Christensen, Mai Choe Lund, Jens Bo Nielsen, Troels Wesenberg Kjaer.
Fig. 1.The location of the EEG and EMG electrode placement according to the standard procedure of the recording of polysomnography[28]. Electrodes on m. Deltoideus, as well as ECG electrodes were also recorded but not included for further analyses. Two examples from two children display the signals for the different sleep stages of the EMG (TA) and EEG (C4). CP, cerebral palsy; TD, typically developing; TA, Tibialis Anterior; SOL, soleus; EEG, electroencephalography; EMG, electromyography; ECG, electrocardiogram. 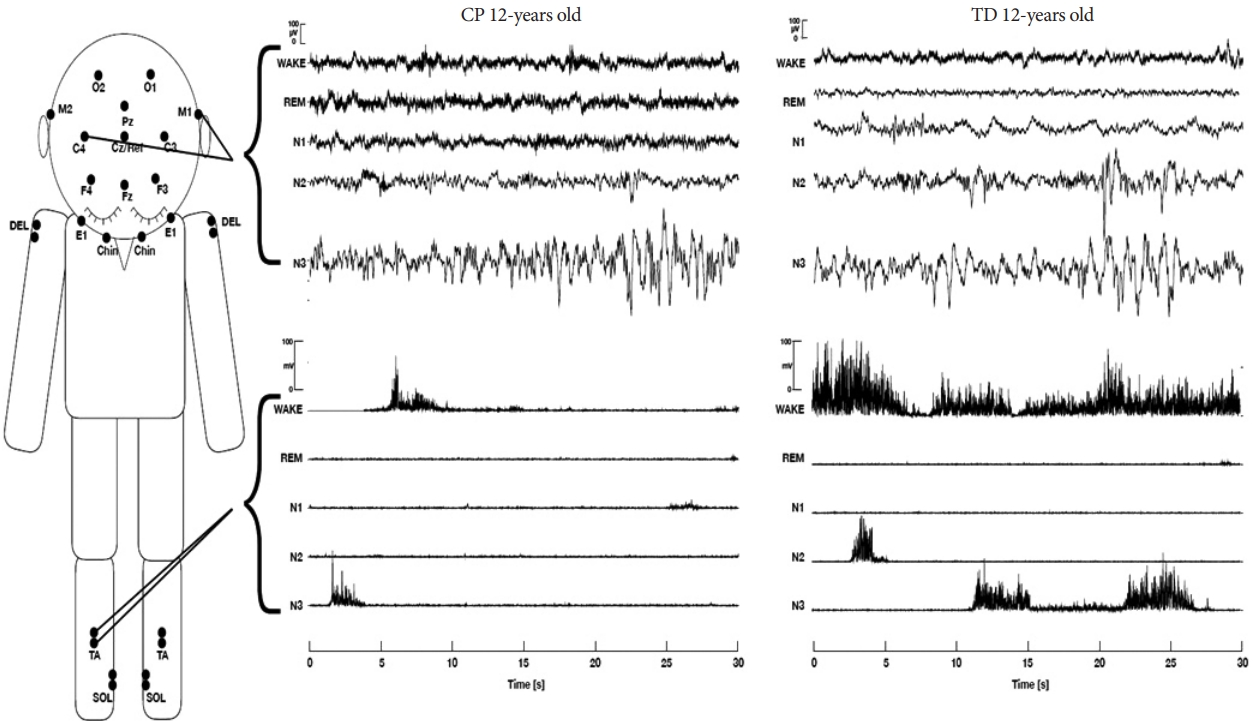
Fig. 2.The average sleep time in the different sleep stages for the CP children and the TD children. X-axis indicates the different sleep stages. Wake describes the total time the children have been awake during the full night recording. The Y-axis indicates the sleep time in percent from sleep onset (from first time N1 was registered in the data) to complete wake up next morning (until the first Wake was registered successively in the data without any other sleep stages following). The p-values are indicated in the table. The significant p-value is indicated on the graph. Error bars indicate SD values. *p<0.05. CP, cerebral palsy; TD, typically developing. 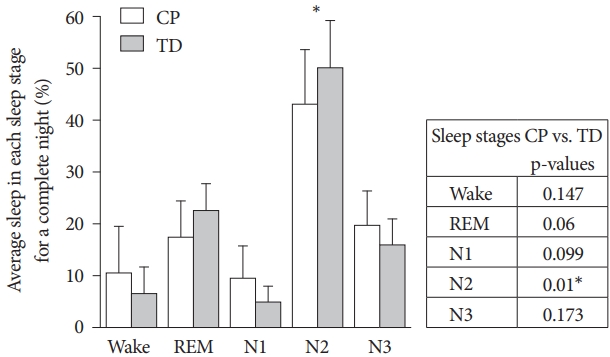
Fig. 3.Muscle activity during the night for TA (A) and SOL (B). The muscle activity is illustrated during the different sleep stages for children with CP divided into least affected side (black) and most affected side (light grey) and TD children (dark grey) respectively in the muscles TA and SOL. X-axes indicate the different sleep stages. Y-axes indicate the value of when muscle activity has exceeded 1SD of averaged activity for a complete night in the individual muscle. Average muscle activity has been calculated for right and left muscles. Every child is marked with a white circle to display the variation. Error bars indicate SD values. *p<0.05. EMG, electromyography; TA, Tibialis Anterior; SOL, soleus; CP, cerebral palsy; TD, typically developing. 
Fig. 4.Results from IMC (A) and CMC (B and C) from the CP children divided into the least (black) and most (light grey) affected side and the average of both legs from the TD children (dark grey). IMC, intermuscular coherence; CMC, corticomuscular coherence; TA, Tibialis Anterior; SOL, soleus; CP, cerebral palsy; TD, typically developing. 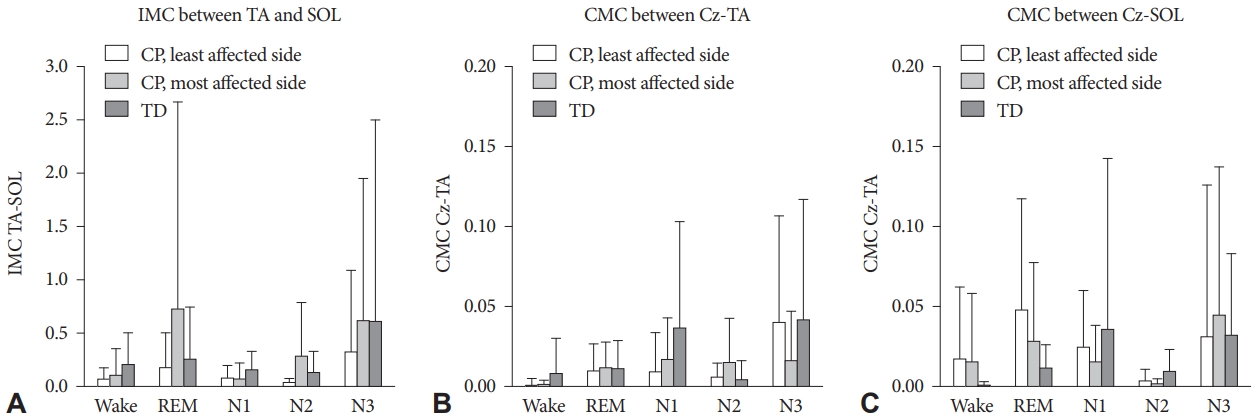
Fig. 5.Representative example of IMC and CMC from sleep stage N2 of the time-series of 30 s from the Cz-electrode, TA EMG and SOL EMG in the center of the figure. In red are displayed the EMG activity that exceeds +1SD of the mean from the EMG activity in the given sleep stage. For EMG-EMG coherence only time periods where both EMG activities exceed 1SD of the mean are used for analyses as indicate by the grey bar between the two time-series. For the EEG-EMG coherence, only the periods where the EMG exceeds 1SD are used, as indicated by the two grey bars between the time-series. To the right are the frequency power of the EEG and two EMG channels used for the subsequent coherence analyses displayed to the left with the cumulant. For analyses of coherence in the different sleep stages and groups of participants, only coherence in the beta band (15–30 Hz) that exceeds the 95% level of confidence is used for the statistical comparisons depicted as the shaded grey area. Furthest to the left are the cumulant densities reflecting at which temporal delays the oscillations of the time-series correlate. IMC, intermuscular coherence; CMC, corticomuscular coherence; TA, Tibialis Anterior; EMG, electromyography; SOL, soleus; EEG, electroencephalography. 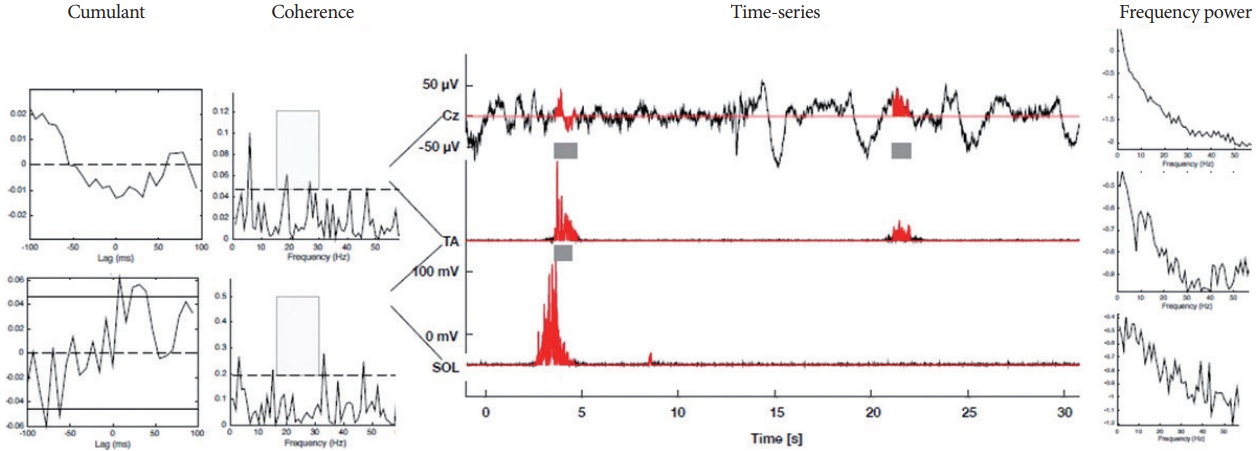
Table 1.Detailed information about all the participants Children were recruited to either CP group or TD group. For the hemiplegic CP children, their most affected side of their body has been noted. Preferred/dominant hand: indicates the dominant arm for the TD children and the preferred arm/less impaired arm for the children with CP based on their diagnosis and few questions from the Edinburgh Handedness Inventory list (Oldfield 1971). MAS which indicate the score on the left (Lt.) and right (Rt.) side of the ankle joint. We did not obtain MAS score for one child in the CP group. GMFCS, Gross Motor Function Classification Scale; MAS, Modified Ashworth Scale; CP, cerebral palsy; TD, typically developing. Table 2.Statistical comparisons for muscle activity during the night for TA and SOL
Linear hypotheses have been made for the TD group between the least/most affected leg in the CP group and within the CP group between least and most affected side. TA or SOL activity = Group-by-SleepStage-by-Affected leg-1 + Age + Sex + GMFCS + (1|Participant). p-values Bonferroni corrected for 15 comparisons. REFERENCES2. Bruni O, Ottaviano S, Guidetti V, et al. The sleep disturbance scale for children (SDSC). Construction and validation of an instrument to evaluate sleep disturbances in childhood and adolescence. J Sleep Res. 1996;5:251-261. https://doi.org/10.1111/j.1365-2869.1996.00251.x.
3. Simard-Tremblay E, Constantin E, Gruber R, Brouillette RT, Shevell M. Sleep in children with cerebral palsy: a review. J Child Neurol 2011;26:1303-1310. https://doi.org/10.1177/0883073811408902.
4. Elsayed RM, Hasanein BM, Sayyah HE, El-Auoty MM, Tharwat N, Belal TM. Sleep assessment of children with cerebral palsy: using validated sleep questionnaire. Ann Indian Acad Neurol 2013;16:62-65. https://doi.org/10.4103/0972-2327.107708.
5. Romeo DM, Brogna C, Quintiliani M, et al. Sleep disorders in children with cerebral palsy: neurodevelopmental and behavioral correlates. Sleep Med 2014;15:213-218. https://doi.org/10.1016/j.sleep.2013.08.793.
6. Zuculo GM, Knap CC, Pinato L. Correlation between sleep and quality of life in cerebral palsy. Codas 2014;26:447-456. https://doi.org/10.1590/2317-1782/20140201435.
7. Lélis AL, Cardoso MV, Hall WA. Sleep disorders in children with cerebral palsy: an integrative review. Sleep Med Rev 2016;30:63-71. https://doi.org/10.1016/j.smrv.2015.11.008.
8. Ghorbanpour Z, Hosseini SA, Akbarfahimi N, Rahgozar M. Correlation between sleep disorders and function in children with spastic cerebral palsy. Iran J Child Neurol 2019;13:35-44.
9. Newman CJ, O’Regan M, Hensey O. Sleep disorders in children with cerebral palsy. Dev Med Child Neurol 2006;48:564-568. https://doi.org/10.1111/j.1469-8749.2006.tb01316.x.
10. Mol EM, Monbaliu E, Ven M, Vergote M, Prinzie P. The use of night orthoses in cerebral palsy treatment: sleep disturbance in children and parental burden or not? Res Dev Disabil 2012;33:341-349. https://doi.org/10.1016/j.ridd.2011.10.026.
11. Horwood L, Mok E, Li P, Oskoui M, Shevell M, Constantin E. Prevalence of sleep problems and sleep-related characteristics in preschooland school-aged children with cerebral palsy. Sleep Med 2018;50:1-6. https://doi.org/10.1016/j.sleep.2018.05.008.
12. Sato H, Iwasaki T, Yokoyama M, Inoue T. Monitoring of body position and motion in children with severe cerebral palsy for 24 hours. Disabil Rehabil 2014;36:1156-1160. https://doi.org/10.3109/09638288.2013.833308.
13. Tardieu C, Lespargot A, Tabary C, Bret MD. For how long must the soleus muscle be stretched each day to prevent contracture? Dev Med Child Neurol 1988;30:3-10. https://doi.org/10.1111/j.1469-8749.1988.tb04720.x.
14. Farmer SF, Sheean GL, Mayston MJ, et al. Abnormal motor unit synchronization of antagonist muscles underlies pathological co-contraction in upper limb dystonia. Brain 1998;121:801-814. https://doi.org/10.1093/brain/121.5.801.
15. Hankinson J, Morton RE. Use of a lying hip abduction system in children with bilateral cerebral palsy: a pilot study. Dev Med Child Neurol 2002;44:177-180. https://doi.org/10.1111/j.1469-8749.2002.tb00782.x.
16. Shortland AP. Muscle volume and motor development in spastic cerebral palsy. Dev Med Child Neurol 2011;53:486. https://doi.org/10.1111/j.1469-8749.2011.03926.x.
17. Willerslev-Olsen M, Choe Lund M, Lorentzen J, Barber L, Kofoed- Hansen M, Nielsen JB. Impaired muscle growth precedes development of increased stiffness of the triceps surae musculotendinous unit in children with cerebral palsy. Dev Med Child Neurol 2018;60:672-679. https://doi.org/10.1111/dmcn.13729.
18. Salenius S, Hari R. Synchronous cortical oscillatory activity during motor action. Curr Opin Neurobiol 2003;13:678-684. https://doi.org/10.1016/j.conb.2003.10.008.
19. Liu J, Sheng Y, Liu H. Corticomuscular coherence and its applications: a review. Front Hum Neurosci 2019;13:100. https://doi.org/10.3389/fnhum.2019.00100.
20. Fang Y, Daly JJ, Sun J, et al. Functional corticomuscular connection during reaching is weakened following stroke. Clin Neurophysiol 2009;120:994-1002. https://doi.org/10.1016/j.clinph.2009.02.173.
21. von Carlowitz-Ghori K, Bayraktaroglu Z, Hohlefeld FU, Losch F, Curio G, Nikulin VV. Corticomuscular coherence in acute and chronic stroke. Clin Neurophysiol 2014;125:1182-1191. https://doi.org/10.1016/j.clinph.2013.11.006.
22. Salenius S, Avikainen S, Kaakkola S, Hari R, Brown P. Defective cortical drive to muscle in Parkinson’s disease and its improvement with levodopa. Brain 2002;125:491-500. https://doi.org/10.1093/brain/awf042.
23. Petrovic J, Lazic K, Kalauzi A, Saponjic J. REM sleep diversity following the pedunculopontine tegmental nucleus lesion in rat. Behav Brain Res 2014;271:258-268. https://doi.org/10.1016/j.bbr.2014.06.026.
24. Ciric J, Lazic K, Petrovic J, Kalauzi A, Saponjic J. Aging induced cortical drive alterations during sleep in rats. Mech Ageing Dev 2015;146-148:12-22. https://doi.org/10.1016/j.mad.2015.03.002.
25. Palisano R, Rosenbaum P, Walter S, Russell D, Wood E, Galuppi B. Development and reliability of a system to classify gross motor function in children with cerebral palsy. Dev Med Child Neurol 1997;39:214-223. https://doi.org/10.1111/j.1469-8749.1997.tb07414.x.
26. Bohannon RW, Smith MB. Interrater reliability of a modified Ashworth scale of muscle spasticity. Phys Ther 1987;67:206-207. https://doi.org/10.1093/ptj/67.2.206.
27. Berry RB, Gamaldo CE, Harding SM, et al. AASM scoring manual version 2.2 updates: new chapters for scoring infant sleep staging and home sleep apnea testing. J Clin Sleep Med 2015;11:1253-1254. https://doi.org/10.5664/jcsm.5176.
28. Wiley ME, Damiano DL. Lower-extremity strength profiles in spastic cerebral palsy. Dev Med Child Neurol 1998;40:100-107. https://doi.org/10.1111/j.1469-8749.1998.tb15369.x.
29. Owens JA, Spirito A, McGuinn M, Nobile C. Sleep habits and sleep disturbance in elementary school-aged children. J Dev Behav Pediatr 2000;21:27-36. https://doi.org/10.1097/00004703-200002000-00005.
30. Hirshkowitz M, Whiton K, Albert SM, et al. National Sleep Foundation’s updated sleep duration recommendations: final report. Sleep Health 2015;1:233-243. https://doi.org/10.1016/j.sleh.2015.10.004.
31. Chaput JP, Dutil C, Sampasa-Kanyinga H. Sleeping hours: what is the ideal number and how does age impact this? Nat Sci Sleep 2018;10:421-430. https://doi.org/10.2147/NSS.S163071.
32. Wayte S, McCaughey E, Holley S, Annaz D, Hill CM. Sleep problems in children with cerebral palsy and their relationship with maternal sleep and depression. Acta Paediatr 2012;101:618-623. https://doi.org/10.1111/j.1651-2227.2012.02603.x.
33. Adiga D, Gupta A, Khanna M, Taly AB, Thennarasu K. Sleep disorders in children with cerebral palsy and its correlation with sleep disturbance in primary caregivers and other associated factors. Ann Indian Acad Neurol 2014;17:473-476. https://doi.org/10.4103/0972-2327.144044.
34. Stickgold R. Early to bed: how sleep benefits children’s memory. Trends Cogn Sci 2013;17:261-262. https://doi.org/10.1016/j.tics.2013.04.006.
35. Cortese S, Ivanenko A, Ramtekkar U, Angriman M. Sleep disorder in children and adolescents: a practical guide. In: Rey JM. IACAPAP e-textbook of child and adolescent mental health Geneva: International Association for Child and Adolescent Psychiatry and Aliied Professions, 2014;1-34.
36. Medic G, Wille M, Hemels ME. Short- and long-term health consequences of sleep disruption. Nat Sci Sleep 2017;9:151-161. https://doi.org/10.2147/NSS.S134864.
37. Fogel SM, Smith CT. The function of the sleep spindle: a physiological index of intelligence and a mechanism for sleep-dependent memory consolidation. Neurosci Biobehav Rev 2011;35:1154-1165. https://doi.org/10.1016/j.neubiorev.2010.12.003.
|
|
|||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||||